Untangling the Nursing Home Knot in Rhode Island
Rising costs, low reimbursements and staff shortages are threatening patient health — and the industry itself. Can we untangle it with new models of care?

Barbara Larivee in her home with a photo of her mother, Dorothy “Betty” Mallon, and a notebook that she used to document her mother’s care in
assisted living and rehabilitation. Photo by Alex Gagne
The traffic was murder, and Valerie Tufano is late for lunch.
Joe Pisano’s green beans and mashed potatoes are cooling on the tray by the time she makes it to the third floor. But he is upright, in a recliner, and that is a victory in itself. Two and a half years ago, Tufano’s brother had a stroke that paralyzed his right side, triggering a cascade of health crises that have required skilled long-term care.

Valerie Tufano and her brother, Joe Pisano, at Cherry Hill Manor Nursing and Rehab Center, where he is monitored closely and has made many health improvements. Photo by Alex Gagne
He lives at Cherry Hill Manor Nursing and Rehab Center in Johnston, and in this moment, he is well. That Joe Pisano is here at all is either a testament to the strength of his spirit, or to Tufano’s advocacy, or to a miracle, or some combination of all three. He has survived severe bed sores, multiple rounds of sepsis and a MRSA infection.
Tufano assesses the untouched food without concern. Pisano eats a full breakfast and most of his dinner. He likes a milkshake, so she whips one up with the ice cream and a protein drink on the tray.
Tufano places the cup in his functional left hand. “Don’t squeeze the cup. Lightly, lightly,” she says.
Pisano’s first nursing home experience, at the Lincolnwood Rehabilitation & Healthcare Center in North Providence, was a disaster, says Tufano. Pisano entered Lincolnwood’s rehab facility in 2022 after an unknown medical event left him unconscious in a tub of overflowing water. He sustained kidney damage and was unable to walk without assistance. After a wandering incident, he was placed in a locked memory care unit, until the end of June, when he suffered the stroke that permanently disabled him.
He transferred to Lincolnwood’s long-term care unit, where his health took a turn for the worse. Tufano says Lincolnwood did not have the staff to properly care for Joe. He needed to spend at least a few hours a day out of bed to improve his balance and prevent bed sores, but spent nearly all of his time in bed, she says. The medical staff had prescribed quetiapine, a strong anti-psychotic drug, to keep him there, she says. Pisano could still swallow, but needed assistance eating. Family members would arrive to find dinner, late, cold and intact.
He lost forty pounds in four months.
“That place was hell — there was never anybody around. He looked like a Holocaust survivor. He was like a zombie in bed. He never got up,” Tufano says. “He was skinny — all bone. All retracted. Knees up in the air. It was just horrendous.”
In the last three years, the Centers for Medicare & Medicaid Services has issued Lincolnwood twenty-three citations and fines totaling $150,621. An investigation into Pisano’s case found the facility deficient for failing to “ensure that residents maintain acceptable parameters of nutritional status, such as usual body weight”; CMS fined Lincolnwood $24,161.
Lincolnwood Administrator Bena Arnett said in a written response that the facility “is committed to providing the highest quality care to the residents we serve. We work proactively, on a daily basis, to continually improve our level of care, just as we did back in 2022 when this resident was under our care during the pandemic.”
How well Rhode Island cares for its 8,000 oldest, sickest and most vulnerable citizens living in the state’s seventy-seven long-term care facilities depends on who you are, where you are and the measuring stick you use.
“Rhode Island is not doing very well,” says Kathleen Gerard of Advocates for Better Care in Rhode Island. She cites the rising number of “immediate jeopardy” incidents — a determination by regulators that an incident, such as giving the wrong medication, has caused or could cause serious harm or death. From 2022 to 2024, they jumped from twenty to forty-three.
“Nursing homes scare people, and it’s easy for people to say that they are bad places. Yet, there are people that have been in facilities for years, their families come and they love it,” says John E. Gage, president of the Rhode Island Health Care Association, which represents sixty-two of the state’s for-profit facilities. “I think the vast majority of residents are very happy with their quality of care.”
Romayne Bono, sixty-eight, knows Royal Health Westerly as a nurse who worked there and as a stroke patient who now lives there. Her care, she says, is “excellent.”
Rhode Island is an old state that is getting older, and there is concern here and nationally that the long-term-care system needs a serious intervention. Since the beginning of the pandemic, nine facilities have closed and thirty-five changed ownership. The ratio of nonprofit and family-owned nursing homes is becoming more lopsided in favor of large corporate chains and private equity owners. Advocates, policymakers and operators are still grappling with a solution.
“If we’re going to deal with our growing population, we really need to look at the health care workforce,” says Maureen Maigret, of the Senior Agenda Coalition of Rhode Island and a former director of the RI Department of Elderly Affairs. “Nursing homes are something everyone should be interested in because we are all going to face something like that, whether it’s for ourselves or our loved one.”
Nursing Home Math
Akshay Talwar was dragooned into the nursing home business in the 1980s, when his physician ex-father-in-law sought his financial advice to manage Briarcliffe Manor Skilled Nursing & Rehabilitation in Johnston. At the time, Briarcliffe was just a nursing home, and Talwar, a former lawyer and CPA, was an associate professor of accountancy at the City University of New York. In the 1990s, Talwar acquired Briarcliffe outright. When he retired from academia twenty-two years ago, he moved to Rhode Island to give it his full-time attention.
“It became a labor of love in there somewhere,” he says. “It was a challenge.”
Long-term care is a highly regulated industry, overseen by federal and state entities. Taking care of medically fragile people is difficult, and the math is complex and daunting. On average, 67 percent of the beds are filled by Medicaid patients — individuals who have exhausted or transferred their financial assets and are supported by government dollars. Medicaid is a federal program, but the size of the budget and how it is allocated is determined by the state. Medicaid reimburses services at a lower rate than Medicare, the federal health insurance program for Americans sixty-five and older, or even Medicare Advantage plans, which reimburse facilities at lower rates than Medicare.
As a person is beset by the conditions that require a nursing home, the care is typically covered by a combination of these payers: Medicare and Medicare Advantage for drugs, short hospital stays and rehabilitation; Medicaid for the rest.
Over four decades, Talwar added 130 private-pay assisted living units, while maintaining a CMS five-star rating for Briarcliff for fifteen years. Talwar says he has been able to keep his stars because his administrative team and much of his care staff have been stable. Financially, he couldn’t do it without those assisted living units at market rates up to $10,000 a month, which supplement the nursing home costs.

Briarcliffe Manor Skilled Nursing & Rehabilitation in Johnston has maintained a CMS five-star rating for fifteen years. Photograph courtesy of Briarcliffe Manor Skilled Nursing & Rehabilitation.
Matt Trimble, CEO of St. Elizabeth Community, the state’s largest elder care and nursing home nonprofit, agrees. St. Elizabeth, which employs 600 people and cares for 2,500, supplements its 122 Medicaid beds with forty-two private-pay beds, four adult day health centers, a home care agency, 153 assisted living units and two federally subsidized senior housing buildings.
“The big problem is Medicaid doesn’t pay anywhere near what it costs, especially since COVID, when labor costs have increased 25 to 35 percent, and Medicaid reimbursement has moved up 14 to 15 percent,” he says.
By law, the state is supposed to reassess its Medicaid nursing home reimbursement rates every three years. But after 2011, it stopped, freezing compensation for more than a decade. In 2023, with the industry pleading for relief, the Executive Office of Health and Human Services hired a consultant to recalculate the rate. In the past, labor — the biggest cost driver — was set at a little bit above the fiftieth percentile of direct costs. The new methodology examined each facility’s 2022 direct and indirect care costs, and set the per diem rate at the fortieth percentile, meaning that a facility spending less on labor than 60 percent of its peers is fully compensated. At the time, thirty facilities were at or below the mark.
“The rationale behind selecting the fortieth percentile incorporated past precedent, nursing facility needs, overall investment and state budget context,” says EOHHS spokesperson Kerri White.
Under the new formula, Governor Dan McKee raised the rates by 14.5 percent and injected $60 million into the system, available last October. John Bonin, the state’s Medicaid deputy director, says EOHHS intends to resume periodic rate reviews.
It was too late to help the nonprofit Linn Health and Rehabilitation, owned by Aldersbridge Communities. The eighty-four-bed, highly rated public-pay facility in East Providence was fifty-three years old when monthly losses of $100,000 forced it to close in July; a General Assembly grant allowed Linn to transition to a public-pay assisted living facility.
“This is where the alarm bells should have gone off,” says Aldersbridge CEO Richard Gamache, a forty-year veteran of the nursing home industry.
Nursing home operators complain that the new formula penalizes facilities that spend more on labor, and the higher labor costs are above the mark, the bigger the gap between costs and reimbursements.
“You’re operating at a significant loss. That’s why you’ve had a lot of facilities close and family-owned homes with good reputations sell to out-of-state corporations,” says Trimble. “If your labor costs are below the fortieth percentile, and you’re getting paid at the fortieth percentile, that’s profit margin.”
Nationally, more than 70 percent of the nation’s nursing homes are operated by for-profit entities, including real estate investment trusts and private equity firms. One study put the national percentage of private equity ownership at 5 percent, but in Rhode Island it’s higher. Tryko Partners, which operates its sixty-five nursing homes through Marquis Health Consulting Services, owns seven facilities here, including Lincolnwood and Elmhurst Rehabilitation & Healthcare Center in Providence, with ratings ranging from zero to four stars. Nationally, Marquis facilities have a below-average CMS 2.2 star-rating.
In the last three years, Elmhurst amassed twelve citations and $654,176 in federal fines. As of February, it had no CMS rating “due to a history of serious quality issues,” and was a part of the Special Focus Facility Initiative, an improvement program for nursing homes with a high number of more serious, and persistent, deficiencies. As of April 2024, Elmhurst was the only such facility in the state, and had not yet met the criteria to graduate to the CMS rating system.
Various studies have noted a relationship between private equity and real estate investment trust-owned facilities and lower staffing levels and more deficiencies. A 2023 federal study compared those entities to other for-profits from 2013 through 2022, and found that private equity investment resulted in a 12 percent decline in registered nurse hours per resident day and a 14 percent increase in their deficiency score index. REIT-invested facilities saw a 7 percent decrease in RN hours and a 14 percent relative increase in deficiencies.
Nurse Stefania Silvestri says her benefits, staffing and the quality declined at the Greenville Center after Genesis HealthCare, one of the nation’s largest nursing home operators, bought it in 2011. In 2021, three private equity firms made significant investments in the chain. During Genesis’s tenure, working with fewer staff and certified nursing assistants became the norm, while the number of patients needing more acute care stayed the same, according to Silvestri.
“I felt like a failure every day — especially during COVID,” Silvestri says. “I would go home and wonder what I could have done better to help a patient be out of bed or just stay alive.”
Long-term care advocate Charlie Galligan moved his eighty-eight-year-old mother to Grace Barker Health in Warren in 2021, after her previous facility was purchased by a private equity firm, accelerating what he says had been a slow decline. The new owners refused to meet with the facility’s family council, and the corner-cutting extended from the thickness of the paper towels to the number of CNAs on the floor.
“My mom was having a rough night, and I didn’t see any CNAs,” he recalls. “I asked at the nurse’s station, ‘How many CNAs are on this wing tonight?’ One of them gave me the hand motion of zero. That was the clincher.”
Other studies have attempted to determine how a tough business with slim margins is so attractive to this sector of owners, by probing the opaque financial arrangements that connect through common ownership of the nursing home to side businesses that act as facility vendors — such as food service companies, pharmacies or labs. These arrangements are legal but there is little oversight on whether their fees are reasonable, and whether staffing suffers as a result. For example, in 2024, researchers published a study of Illinois facilities from 2000 to 2021, finding that 77 percent were transacting with related parties for real estate or management services, resulting in 20–25 percent increases in total costs.
At the time of acquisition, the RI Department of Health’s Health Services Council reviews the buyers and related parties providing services; DOH makes the final decision. But some believe the financial reporting should be more robust and ongoing.
This session, the DOH proposed a measure that would ensure that nursing home revenue was being invested in resident care, and prevent nursing home owners from withdrawing more than 3 percent of their total reported annual revenue in any given year without their approval. Senator Dawn Euer (D- Dist. 13, Newport and Jamestown) was a sponsor of a financial transparency bill, which would define related parties and require annual audited financial statements.
“We are trying to get to that question: Where is all of that money going to and how is it being allocated?” she asks. “We want to make sure we are getting the full financial picture.”
Staffing Conundrum
Barbara Larivee lays a photo of her mother Dorothy “Betty” Mallon on her kitchen table. Taken on St. Patrick’s Day 2024, her ninety-five-year-old mother is resplendent in kelly green. Up until she was ninety, Mallon drove, played golf and was a foster grandparent at Myron Francis Elementary School in Rumford. In 2023, macular degeneration and the onset of dementia forced Mallon into assisted living, where she did well — until she fell, fracturing her tibia.

Barbara Larivee advocated for her mother’s health in assisted living and rehabilitation by documenting incidents in a notebook and taking photos of her condition. Photo by Alex Gagne
Larivee pulls another colorful photo from a sheath. This one from January is of purple swollen shins, and another of an inflamed pink tongue with clusters of white pustules.
The last fifteen weeks of Mallon’s life were an ugly physical breakdown that Larivee documented in a notebook, as Mallon moved from assisted living to rehabilitation, back to assisted living, and finally to Elmhurst. It’s a diary of small indignities such as dirty dentures and inadequate toileting and instances of serious inattention, staff shortages and dropped communications that allowed Mallon’s ailments to fester. Larivee documented the pressure sores that developed on her mother’s heels, the lower legs that ballooned beyond the capacity of her socks, the untrimmed toenails that grew into her skin; she left Elmhurst with a painful-looking case of oral thrush.
“It was horrible. I told one of her nurses everything. She looked at me and said, ‘How come you didn’t call a lawyer?’ I said, ‘Because that’s not what it’s about. I want people to know: Be active in your loved ones’ care so that it’s done right.’”
After three weeks at Elmhurst, Larivee engaged hospice services, rented a hospital bed and brought Betty Mallon home.
“I put on 1940s music, made whatever she wanted to eat. I did her wound care and sponge-bathed her. We joked; we laughed. I made sure my mother had the best rest of her life and she died clean, with dignity and respect.” Larivee choked up. “Those places should be ashamed of themselves.”
Responding to a Rhode Island Monthly inquiry, Administrator Lindsey Bouchard wrote: “Elmhurst was not subject to any regulatory actions during the time period referenced. We take every resident concern seriously and work hard to improve our qualitative and quantitative standards of care.”
Lawmakers, labor and advocacy groups believe there would be fewer such stories with more staff and better pay for CNAs. In 2021, the General Assembly thought it had solved the crisis with the passage of a bill mandating minimum staffing levels and funding for higher direct care staff wages. The Nursing Home Staffing and Quality Care Act required nursing homes to provide 3.81 hours of resident care per day by January 2023. The law strictly defined the care providers making up those hours; the penalties for noncompliance were stiff. Facilities could be fined up to 300 percent of those missing staff hours. Repeat offenders would lose their Medicaid funding.
The bill solved nothing.
The RIHCA, which failed to persuade the legislature that it had written what operators considered an industry suicide pact, turned to McKee. The governor delayed implementation, and in December 2023, issued and later renewed an executive order that stayed the fines.
“It was an unfunded mandate implemented in the midst of the pandemic when our workforce was already down 20 percent; 87 percent of Rhode Island nursing homes are out of compliance,” says Gage. “In the first quarter of enforcement [the fines] would have been $19 million and over the course of four quarters more than $100 million.”
The legislature then passed the Workforce Standards Board bill, which created an advisory board to make recommendations on staffing, wages and training, set minimum wage and working standards and assist in compliance. McKee vetoed the measure, saying that it would not provide a comprehensive solution.
“It is critical that we have a roadmap for the future, and that’s why we called for a State Health Care System Planning Cabinet that takes a unified approach across all our health and human services agencies to, among other things, develop a vision for how we can best support our older adults and anyone else in need of long-term care,” McKee said in a written statement.
“The lesson learned was that we have to be flexible and cognizant of the environment,” says House Speaker K. Joseph Shekarchi. This session, he says, everything is on the table, “and I think you’ll see a willingness for everybody to sit down and work together.”
In the meantime, under the Biden administration, the CMS finalized a regulation that set minimum staffing levels to a total of 3.48 hours per resident, per day of nursing care delivered by a combination of RNs, CNAs and LPNs. The April 2024 rule also requires states to collect and report on the percent of Medicaid payments that are spent on compensation for direct and indirect care workers.
Advocates believe the Trump administration will kill it. Gage says the American Health Care Association is lobbying for that.
Shekarchi worries “that if Trump decides to stop or cut Medicaid payments, we’re going to be in real dire straits, because we don’t have anywhere near that amount of federal money to make up with state funds. That keeps me up at night.”
Toward a Better Future
Tony Russo, freshly showered, is breakfasting in his bedroom at St. Elizabeth’s Green House 15: Rice Krispies with blueberries in his bowl and Italian crooner Jimmy Roselli on the radio. Liz Mora is in the open-concept kitchen, laying cod fillets in a pan to accompany a lunch of orzo, creamed spinach and spice cake. Other residents watch television in the large den. The vibe is laid back this Sunday morning.
Russo, just shy of ninety-nine years old, came to East Greenwich’s Green House in May. He calls the place homey, and the help “terrific. They are always there for you.”
In 2017, St. Elizabeth became the first — and only — facility in the state using the Green House model of skilled nursing care. Developed by the Green House Project, this approach replicates residential living in a nursing home. Since 2003, the organization has helped create nearly 400 Green Houses in the U.S. and Australia.
Each Green House at St. Elizabeth houses twelve residents, overseen by cross-trained CNAs and nurses called Shahbaz, a Persian word for falcon. In addition to their usual duties, the Shahbazim cook, do laundry, housekeep and act as companions to the residents. The four tastefully landscaped homes would fit neatly in any up-market suburban neighborhood. The interiors resemble a high-end hotel, with airy bedrooms and private bathrooms.
Saint Elizabeth started this project with a $4.5 million capital campaign and DOH’s permission to add forty-eight new nursing home beds, ending a twenty-five-year moratorium. The monthly fee is $8,000, and when it opened, the population was a mix of public and private payers. Recently, St. Elizabeth switched to private payers to offset rising costs.
Aldersbridge CEO Gamache says it’s time to consider other affordable options. Linn Health successfully transitioned a third of its former skilled nursing residents. That cohort — dementia patients who needed the assistance of a caregiver to get through the day — had wound up in a nursing home because the families couldn’t afford private-pay assisted living.
Initially, Gamache was surprised it could be done.
“I thought wow — our acuity must be very low compared to the average nursing home. But we were right in the middle. One third of our people could be cared for in a lower cost-setting if it was available, so theoretically, all nursing homes are likely to have people that could be cared for this way,” he says. “That’s one light at the end of the tunnel.”
He is also a part of the Live Oak Project, a national group of advocates reimagining the delivery of long-term care. Talwar modestly would like to see government support for capital improvements desperately needed to modernize the nation’s aging facilities, but he isn’t sure the policymakers have enough imagination to reform the entire system.
“The need is going to grow. Exactly what the model is to fulfill that need in the next five to twenty years will depend on policymakers. And they need to think hard instead of adding rule upon rule, year after year. If people could solve these problems by rule-writing, the problems would have been solved. It needs a fresh start,” he says. “But I just don’t know anymore. We’ve got ourselves in so many different knots.”
The state has also been working on keeping people out of long-term care altogether. The Hospital Care Transitions Initiative program has tried to return more than 1,000 patients to home care, with a 75 percent success rate. Office of Healthy Aging Director Maria Cimini says the state is “taking proactive steps” to meet the need “by expanding home and community-based services, improving caregiver support, and strengthening policies that promote aging in place.”
Tufano moved Pisano to Cherry Hill around Thanksgiving 2022. He’s gained weight, he’s alert, he’s off of the quetiapine and has his own nurse practitioner who monitors him closely. Pisano is a complex case, given his paralysis, dementia and a Foley catheter which can lead to infections. Tufano, a RN, pushes the staff to be proactive, and commended their handling of a recent incident, in which they immediately notified Tufano that Pisano was ailing and started treatment.
“I was really proud of them, because they were trying to keep him out of the hospital,” she says.
Tufano and her younger brother weren’t close growing up, but they are now. She spends hours each week by his side.
“Hey!” Pisano says loudly. He is not very verbal, and yet he can make some of his needs known. He reaches for his sister’s hand.
“Are you trying to tell me something? I’m listening,” Tufano says.
Tufano is part of an informal group of third-floor caregivers, who keep an eye out for each other’s loved ones and get in touch if anything’s amiss — that helps. And the staff “are nice, but they think their lives should just go as they are,” she says. “Me as a family member, I put a lot more effort into it.”
Some think Tufano is “delusional” for working so hard to keep him going, she says. She watches Pisano enjoy his milkshake.
“My brother’s very strong. He’s almost lost his life three times, but he comes back. What is his quality of life?” she asks. “I don’t know. He wants to live.”
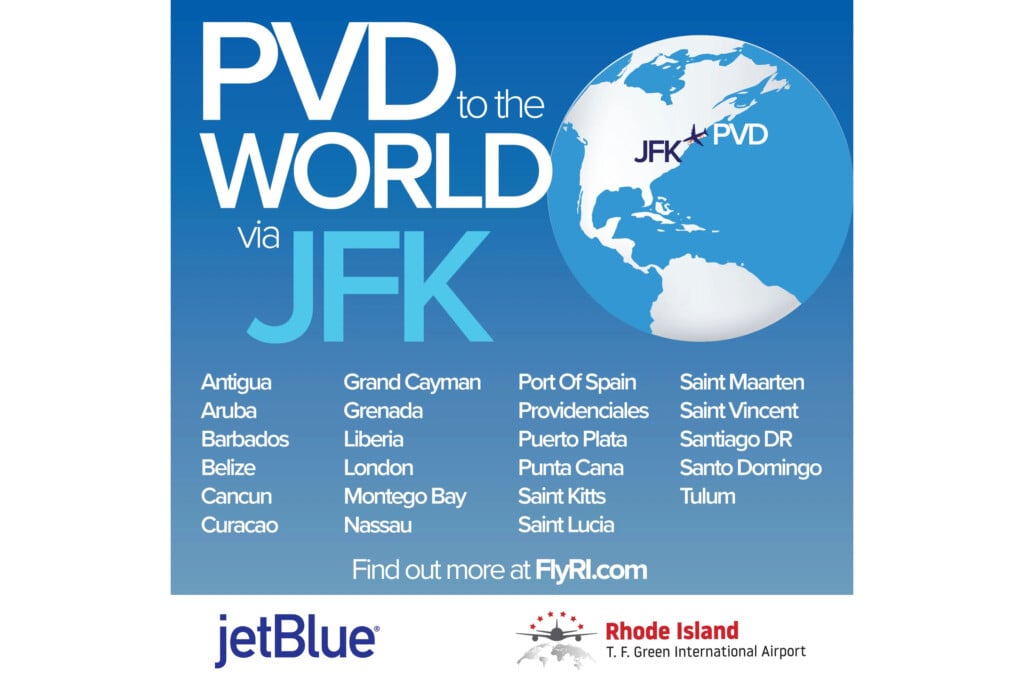
Explore Nursing Home Ratings
CMS assigns nursing homes one to five stars annually, based on three metrics: the last three years of its health inspections; staffing, measured by RN and CNA care hours and staff turnover; and other quality measures, such as “if residents have gotten their flu shots, are in pain, or are losing weight,” according to the CMS website. Ratings are fluid and change if circumstances warrant. This information is publicly available at the “Compare Care” webpage at medicare.gov/care-compare/?providerType=NursingHome. You can search a specific facility by name, or search “Rhode Island” for all nursing homes in the state. Each facility’s webpage contains the star rating for each metric, the last three years’ inspection and deficiency reports and information about fines.
Nursing Homes: By the Numbers
8,000 — Number of residents in long-term care in Rhode Island.
77 — Number of long-term care facilities.
67% — Percentage of beds filled by Medicaid patients.
70% — Percentage of the nation’s nursing homes that are operated by for-profit entities, including real estate investment trusts and private equity firms.
3.48 — The CMS-regulated set minimum of total hours, per day, per resident of nursing care delivered by a combination of RNs, CNAs and LPNs.
24% — In 2023, the percentage of the population that was aged sixty or older.
2.7% — In 2023, the percentage of the population that was aged eighty-five or older.
100% — Increase in the number of residents aged seventy-four to eighty-four by 2040.
72% — Increase in the number of residents aged eighty-five-plus by 2040.